
Nonjudgmental and Patient-Focused Healthcare for Bears with Dr. Justin Penny
The only thing better than one bear doctor is two, amiright?!
When I came across Dr. Justin Penny on Instagram, I immediately reached out, hoping he’d be willing to share his expertise with us a both a doctor and a member of the bear community just as Dr. George Forgan-Smith has done for us for the last year and a half. I am pleased to say that he generously and enthusiastically agreed to be a medical consultant for us and just like with Dr. George, we will be bringing medical issues relevant to our community to his doorstep for advice from time to time. The plan is to alternate between Dr. Justin and Dr. George because, well, I have a million questions and bear health and wellness is always top of mind for us at Bear World Magazine.
Before we dive into the medical issues, however, I thought it prudent to properly introduce you guys to Dr. Justin with a Q&A covering his career, medical training and experience with the bear community.

John Hernandez (JH): Hi Dr. Penny, thank you for joining me. What area of medicine do you practice and what do you consider your area of expertise?
Dr. Justin Penny (Dr. Justin): I’m kind of the Renaissance man of doctors (laughs). I’m a full spectrum family physician. I do academic medicine; I teach residents and medical students; I work in a clinic where I’m a primary care physician and I work in the hospital where I make rounds on my adult patients. I also do obstetrics and labor & delivery. I get to deliver babies!
My content expertise is LGBTQ+ medicine and primary care. I do transgender care including hormones for adults and adolescents. I’m continuing to get training to do puberty suppression. And on top of that, I also do bioethics where I am a consultant for local hospitals doing consults on difficult cases. I like to be the kind of generalist that knows a lot about a lot, but as soon as I get to the edge of my understanding or ability, that’s when I refer to the specialists.
JH: Wow, what a slacker! (Laughs) Just kidding of course. That’s incredible. Tell me about your medical training and where you went to school.
Dr. Justin: I grew up in Kentucky. I did two undergrad degrees at the University of Kentucky, biology, and classical studies focusing on architecture, art, history of the ancient world. Then I went to Kansas City for medical school, earning my DO which is a Doctor of Osteopathic Medicine. About 20% of physicians in the United States are DOs, you may have met a DO and never known it and just thought they were another MD. DOs get a ton of extra training in musculoskeletal medicine, where we can use our hands to treat acute and chronic conditions, including pain. So, for instance, if you come into my office and have back pain, I can evaluate it, figure out if you need x-rays, but also use my hands to treat pain.
When I was in medical school I did my masters of ethics as well. Because I said “ohh medicine’s not hard enough might as well get a master’s at the same time”. (Laughs) I graduated medical school in 2017, then I came up here to Minnesota where I completed residency in family medicine. After that I completed my MD boards; then because I wanted to keep my osteopathic medicine part, I also did the DO boards in both family medicine and osteopathic manipulative medicine. I have a journey of collecting a lot of very expensive pieces of paper. (Laughs)

JH: In addition to everything else you do you’re a clinical ethics assistant professor and a member of your local clinical ethics consultant team. Just what is clinical ethics and what is bioethics?
Dr. Justin: Bioethics is a field where one can be a PhD philosopher. One could come to ethics through nursing or clinical care medicine like I did, or law. And it’s an extra set of training to really help care teams and patients and families explore difficult conversations. There is some formal training where we look at current philosophy that might have been developed years ago, or different models of philosophy that help answer complex questions.
For example, if there is a loved one on a ventilator, and one child says “they would have never wanted this,” and the other says “they’re a fighter,” who gets to decide the goals of care for that patient because they can’t speak for themselves? Are there processes that were set up in advance? So, it may include care planning, living wills, documents that might have been overlooked or if not we can help navigate the situation to really help a patient speak for themselves even when they can’t.
A lot of people don’t really understand what ethics, this big amorphous topic, is. But they do understand some of the main principles of ethics: autonomy, which means the ability to self-govern; nonmaleficence which is that do no harm thing that doctors and a lot of care professionals have in their codes of conduct; beneficence which is do the right thing or do the thing that would help people. And then justice, which is that idea of weighing resources, such as if we have 15 people that need a ventilator, but we only have five ventilators available. That’s where certain political parties might call ethicists death panels; but other people who understand the field might say that we help care teams navigate these difficult conversations, and we take that sole responsibility off of somebody when they have this overwhelmingly difficult choice.
JH: That’s a tough situation to be in. Thanks for that clarification. What would be some of the intersectionality between like LGBTQ care and ethics? What kind of situations arise in that area?
Dr. Justin: I think right now it’s access to care, especially across the United States, but it’s not only the United States. The NHS in England is trying to limit access to care for trans adolescents and even transgender adults. Anytime you’re thinking about allocation of resources or barriers to care, that’s a justice issue. As a writing experiment my students would argue that it’s harmful, so that’s maleficence. They could argue that patients and families have limited choice and or have their hands tied, so that’s limiting autonomy. But overall, we think of access to care as a justice issue where there is an outside entity limiting resources that maybe even clinicians and providers want to provide, but now the state is coming in saying we can’t do certain things. There’s been a lot of talk about puberty suppression, but also some laws coming out throughout the South (US) that are limiting access to mental healthcare. I think it’s really hard to claim that that’s in a child’s best interest if you’re trying to limit access to mental healthcare.
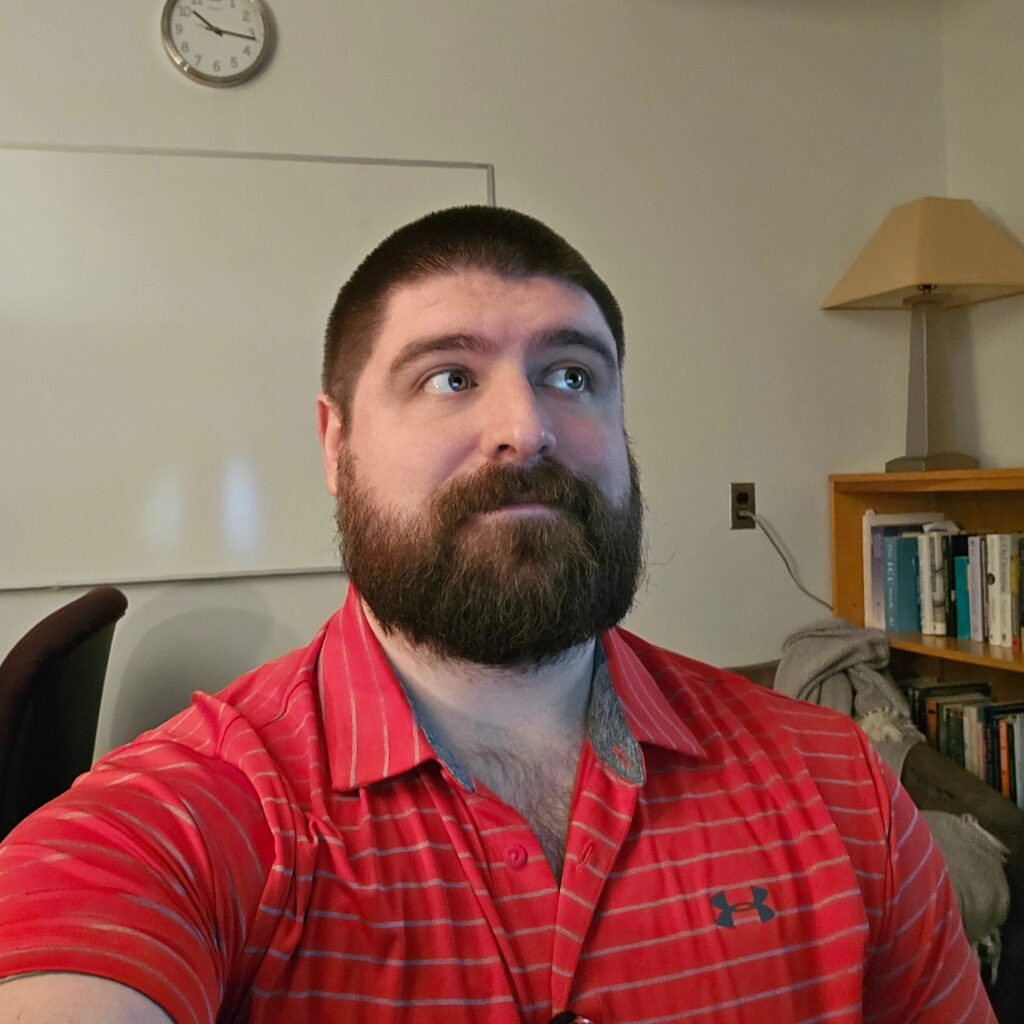
JH: I think you’re right about that. Now since we are a bear magazine I have to ask; do you identify as a bear? Do you hang out in the community or attend bear events?
Dr. Justin: I do. I am in the community. I’m on queer social media. I go to events. It’s funny because my husband is also a physician. I go by Doctor Bear, that’s my nickname. A lot of people know us as that young doctor couple. I think our first bear event was probably TBRU in maybe 2015 when I was still in Med school. Friends and I for some reason had a lucky weekend off and just went down and it was just such a welcoming experience. Growing up gay, I feel like I didn’t have that representation in media, in culture. I didn’t know that being gay you could also be a larger body person, or a person with hair, or a person that just didn’t have this, you know, 1990s chiseled esthetic. I didn’t actually really come out until medical school, and as soon as I came out, I found community in Kansas City and started to really just embrace who I was and came into the scene, if you will.
JH: What do you think are the biggest health concerns for the bear community in your opinion, from what you’ve seen?
Dr. Justin: I think that society might say weight. But I would challenge that and say that I think our community thinks more about mental health. I think that our community might say things like substance abuse. This is where representation to me matters and a lot of my patients have established trust with me not only because I’m an openly queer poly human in the world, but I am a bear. And they’re like, I’m a big guy, I want to go see a big guy. I very rarely talk about weight in a clinical setting unless my patient wants to.
And are there relationships between weight and cardiovascular health? Maybe. But no matter how much weight you carry or your size, it’s more about if you are you able to go up two flights of stairs? Are you able to do the activities that bring you joy? Are you able to move around in the world and feel good? If you’re able to do that, then I don’t care what the number on the scale says. I care more about your blood pressure than the number on your scale.
My care philosophy is really creating that partnership with the patient and their loved one, if they’re involved in that decision making, to explore their goals and values. That’s where I bring my ethics and I do a lot more of a goals and values-based care approach to medicine. So, if your biggest concerns are your mental health, then great, let’s figure out if we can support your environment, figure out what your stressors are, and connect you with a psychologist or therapist that can really help you explore. And then if medications are within your goals, I’m happy to prescribe medications. But if that’s not within your goals, then let’s figure out how to get to your goal without me interjecting something that you don’t want.
If readers get one thing from this, I would want them to get that there are nonjudgmental and kind doctors out there and if you don’t feel like you can talk about sex, for instance, or about any of your concerns with your doctor, get a new doctor. There’s lots of lists out there. There’s telemedicine that can provide a bridge to an in-person doctor until you find one. There’s just so many options, and especially because I’m training students and residents, we are changing how we’re teaching new doctors. You just have to look, ask the community and figure out who your friends see and go see them.

JH: That advice is worth its weight in gold and thank you for saying that Justin. And with regards to sexual health, are there any kind of sexual health factors that you think bears and gay men in general should be on the lookout for currently?
Dr. Justin: I think the most important thing around sexual health is just being open with communication and testing. There’s always been a lot of stigma and a lot of fear around disclosing positive test results to partners. We can’t control other people’s reactions, but it’s still the right thing to do to let your partners know to get tested if there is anything that came up with a positive result and recommitting to routine testing. If you’re on PrEP, that should be every three months and maybe more often depending on number of partners. If you’re using PrEP on the 2-1-1 dosing, which is an intermittent dosing, then maybe that makes sense every six months for that individual, but just committing to routine testing is the key.
JH: Well Doc, you’ve already given me a ton to think about. Thank you so much for taking the time out to do this interview and to help me out with future medical articles.
Dr. Justin: My pleasure!








Love this! That’s why he’s my kid’s Guncle. Keep rocking it Justin, representation matters!
Gorgeous sexy beast! Doctor Bear. XXX
Love the contrast between the US point of view here and George’s Australian POV.
Given all his copious free time, he should come to Easton Mountain and teach on Bear Medical Ethics!
LOVED this interview!!!